
On June 24, the U.S. Supreme Court overturned Roe v. Wade. By undoing the landmark 1973 decision that protected a person’s right to an abortion, the highest court in the country has shifted decisions about this medical care to individual state and local governments.
Some states have already passed laws that curtail abortion access. Now, without the federal protections Roe v. Wade provided, other states will likely follow suit.
Many of those legislative efforts invoke medical and scientific language, in an effort to define when life begins. Heart development, fetal pain and viability have all been brought into justification for abortion restrictions. But many of these rationales don’t line up with the biology of early development. Texas’ 2021 “heartbeat law,” for instance, bans abortion after about six weeks when heart cells purportedly begin thumping. At that early stage of pregnancy, there isn’t yet a fully formed heart to beat.
Like most aspects of biology, early human development involves many complex processes. Despite the rhetoric around these issues, clear lines — between having a heart and not having a heart or being able to survive outside of the uterus — are scarce, or nonexistent.
“There aren’t these set black-and-white points for much of this,” says obstetrician-gynecologist Nisha Verma, a fellow with the American College of Obstetricians and Gynecologists in Washington, D.C.
Here’s what’s known about five key aspects of pregnancy biology that often come up in abortion debates.
1. The early timeline of a pregnancy is easy to misunderstand.
That’s because how dates are determined is supremely confusing. The standard pregnancy clock actually starts ticking before a sperm cell encounters an egg, two weeks before, on average. An ovary releases an egg around day 14 of an average 28-day menstrual cycle (SN: 6/19/21) . (Day 1 is the first day of menstruation; day 1 is also when a pregnancy officially begins in the month an egg is fertilized.) That means that when a sperm fertilizes an egg, a person is already officially two weeks pregnant. As nonsensical as that sounds, it’s the simplest way medical professionals can date a pregnancy.
That timeline means that abortion bans at six weeks, enacted in Texas, Oklahoma and Idaho, take effect earlier in pregnancy than many people think, Verma says. In 2020, she surveyed people in Georgia, where she was practicing medicine at the time, about their understanding of the timing. “Some people will say the six weeks is after your first missed period,” she says. “Some people think it’s from the date of conception.” Neither is correct.
The ban would start four weeks after fertilization. Counting back, that’s two weeks after a missed period, which is often a person’s first indication that they might be pregnant. Such bans leave a person very little time — two weeks after a missed period — to access an abortion.
What’s more, these dates are based on averages. Many women have irregular menstrual cycles. Birth control isn’t 100 percent effective, and certain types can eliminate menstruation altogether, throwing even more uncertainty into the early timeline of pregnancy.
2. Pregnancy takes more than sperm meeting egg.
That meeting, which usually takes place in one of the two fallopian tubes near the ovaries, is fertilization, a process in which two cells fuse and mingle their genetic contents, creating what’s known as a zygote (SN: 1/10/15). But a fertilized egg does not automatically lead to a pregnancy, says obstetrician and gynecologist Jonas Swartz of Duke University School of Medicine. “Equating them doesn’t make sense from a medical standpoint.” Up to 50 percent of fertilized eggs do not implant in the uterus, researchers have estimated.
The genetic material needs to combine in the right way. The growing ball of cells needs to travel to the uterus and implant itself in the right spot. And the right balance of hormones need to be churned out to support the pregnancy. “There are so many things other than the sperm meeting the egg that actually matter for this to become a pregnancy that has a chance to develop further,” says Selina Sandoval, an obstetrician and gynecologist who specializes in complex family planning at the University of California, San Diego.
Lawmakers in some states are considering abortion rules that apply to a fertilized egg; Oklahoma had already passed such a law. That includes fertilized eggs that lodge in the wrong spot, the fallopian tube, for example. Called an ectopic pregnancy, this can lead to life-threatening medical emergencies when the growing tissue ruptures the tube and internal bleeding ensues. “These are pregnancies that under no circumstance can become a healthy pregnancy,” Sandoval says. “In fact, if they aren’t treated and continue to grow, they will kill the patient.” Laws that apply to a fertilized egg could “limit our ability to treat patients for ectopic pregnancies,” she says.
3. “Heartbeat laws” are not what they seem.
A Texas law bans abortions “after detection of an unborn child’s heartbeat.” But the rhythmic sounds heard on an ultrasound early in pregnancy aren’t caused by the opening and closing of heart valves as they move blood through the heart’s chambers, the motion that produces a typical lub dub sound. That’s because those chambers haven’t yet developed. On early ultrasounds, the heartbeat-like sounds are created by the ultrasound machine itself.
“What we’re seeing is actually the primitive heart tube and the cells in that heart tube having electrical activity that causes fluttering,” Verma says. “The ultrasound is actually manufacturing that sound based on the electrical activity and fluttering motion.”
Using the term “heartbeat” to describe the fluttering makes sense in some situations, like in conversations with excited parents-to-be, Verma says. “I’ve taken care of countless people who have seen that first ‘heartbeat’ on ultrasound for a desired pregnancy, and it’s this huge, exciting moment,” she says. “I don’t want to be dismissive of that.” She says two things can be true at the same time: “It can be exciting for a patient. It also isn’t a scientific thing.”
4. Fetal pain is difficult to define.
A bit of biology that’s often used to restrict abortions is the claim that fetuses (which form at week 11 of pregnancy) feel pain.
“Pain is very complex,” Swartz says. “It requires not just a physical response, but the ability to suffer as a result.”
Knowing what a fetus experiences is impossible, but brain development studies provide some clues. The experience of pain starts with the senses detecting something noxious. Those signals then have to travel to the cortex, the outer layer of the brain that helps interpret that sensation. In human fetuses, those brain connections don’t exist until about week 24 or 25 of pregnancy. In guidelines written by members of the Society for Maternal-Fetal Medicine, researchers write that these connections are necessary for the experience of pain, but are not sufficient on their own to conclude that pain is possible.
In human fetuses, these connections aren’t actually operational until about week 28 or 29 of pregnancy, other studies suggest. “We can say with really, really good confidence that no sooner than 28 weeks is [pain] even possible,” Sandoval says.
The vast majority of abortions — over 90 percent — happen in the first trimester, before week 13 of pregnancy. The number of abortions after 24 or 25 weeks is “vanishingly small,” Swartz says.
5. When a fetus could survive on its own is a complex medical calculation.
The word “viability” is often used as a sharp cut-off point to mark the age at which a fetus could survive outside of the uterus. The problem is that one clear cut-off does not exist.
“That has been a moving line as science has advanced and our ability to support very small babies has advanced,” Swartz says. “But it’s also not a fixed line for babies born now.”
On average, babies born around 22 to 24 weeks gestation either don’t survive or they survive with major health problems. Whether a fetus will survive if delivered depends on a whole suite of other factors, Swartz says. They include fetal sex, weight, developmental issues and mother’s health, not to mention individual health care facilities’ capabilities and training.
The American College of Obstetricians and Gynecologists recently removed mentions of “viability” in their guidance on abortion care. “It’s such a complicated concept that we can’t make blanket statements about it,” Verma says. “It’s something that needs to be left to the clinician looking at the patient.”
Inaccurate descriptions of biology can influence restrictions around reproductive health, and as a result, the health care people are able to receive, Swartz says. A colleague of his, for instance, wasn’t able to get appropriate medical care when she experienced signs of a pregnancy loss. Because of state abortion restrictions, her physician decided to delay treatment, an emotionally distressing experience she wrote about last year in Obstetrics and Gynecology. Abortion regulations based on flawed medical and scientific premises, Swartz says, “places priority on a potential life over the actual life of the person sitting in front of me.”
 A new treatment could restore some mobility in people paralyzed by strokes
A new treatment could restore some mobility in people paralyzed by strokes 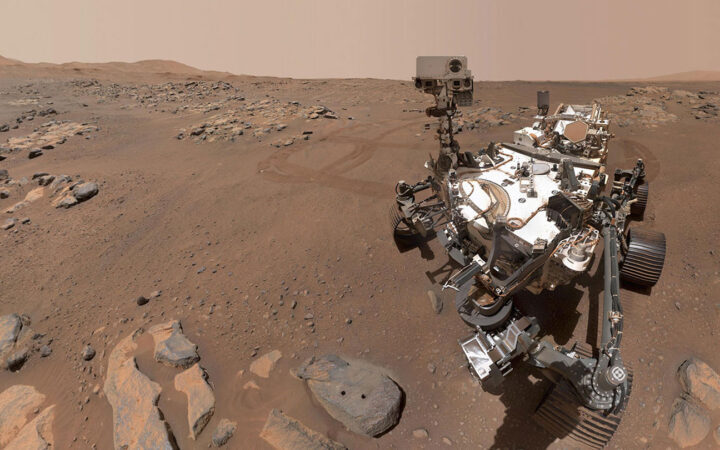 What has Perseverance found in two years on Mars?
What has Perseverance found in two years on Mars? 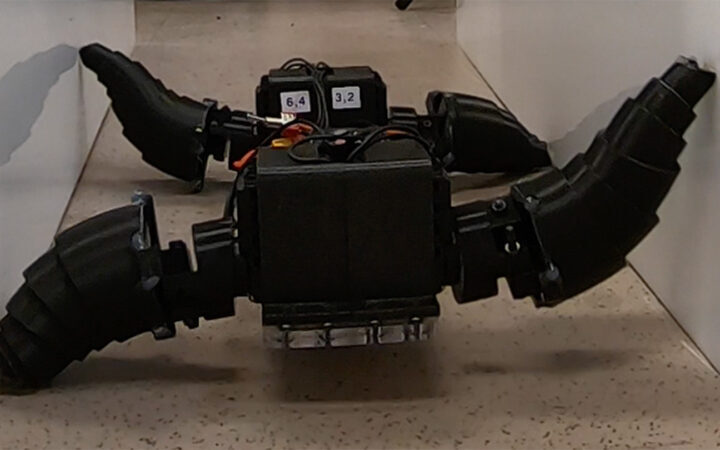 This robot automatically tucks its limbs to squeeze through spaces
This robot automatically tucks its limbs to squeeze through spaces  Greta Thunberg’s new book urges the world to take climate action now
Greta Thunberg’s new book urges the world to take climate action now  Glassy eyes may help young crustaceans hide from predators in plain sight
Glassy eyes may help young crustaceans hide from predators in plain sight 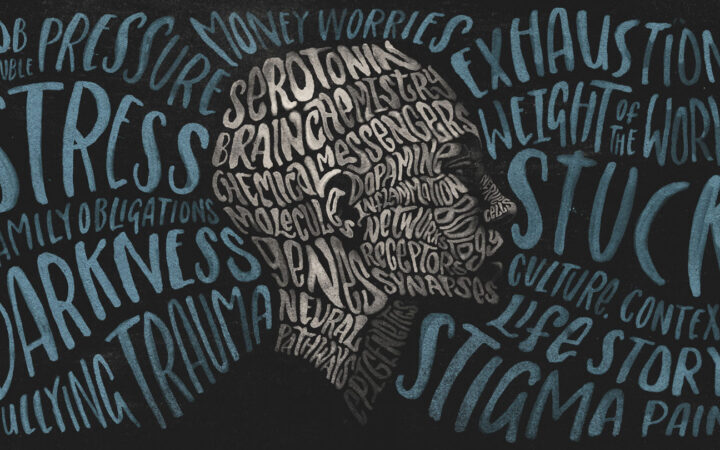 A chemical imbalance doesn’t explain depression. So what does?
A chemical imbalance doesn’t explain depression. So what does?