
Not long before the end of the school year, my husband and I received an e-mail from our fifth-grader’s principal that may now be all-too-familiar to many parents. The subject line included the words, “MULTIPLE COVID CASES.”
Several students in my daughter’s class had tested positive for COVID-19. Her school acted fast. It reinstated a mask mandate for 10 days and required students not up-to-date on their COVID-19 vaccinations to quarantine.
These precautions may have helped — my daughter didn’t end up bringing the virus home. But for kids who do, COVID-19 can hopscotch through households, knocking down relatives one by one. And it’s not clear how long one infection protects you from a second round with the virus.
Recent high-profile cases have put reinfections in the spotlight. Health and Human Services Secretary Xavier Becerra has had two bouts of COVID-19 in less than a month. So has The Late Show host Stephen Colbert. Back at his desk in May, he joked, “You know what they say. ‘Give me COVID once, shame on you. Give me COVID twice, please stop giving me COVID.’”
Just a few months ago, scientists thought reinfections were relatively rare, occurring most often in unvaccinated people (SN: 2/24/22). But there are signs the number may be ticking up.
An ABC News investigation that contacted health departments in every state reported June 8 that more people seem to be getting the virus again. And omicron, the variant that sparked last winter’s surge, is still spawning sneaky subvariants. Some can evade antibodies produced after infection with the original omicron strain, scientists report June 17 in Nature. That means a prior COVID-19 infection might not be as helpful against future infections as it once was (SN:8/19/21). What’s more, reinfection could even add to a person’s risk of hospitalization or other adverse outcomes, a preliminary study suggests.
Scientists are still working to pin down the rate of reinfection. Like most questions involving COVID-19 case numbers, the answer is more than a little murky. “You really need to have a cohort of people who are well followed and tested every time they have symptoms,” says Caroline Quach-Thanh, an infectious diseases specialist at CHU Sainte-Justine, a pediatric hospital at the University of Montreal.
A recent look at hundreds of thousands of COVID-19 cases among people in the province of Quebec found that roughly 4 percent were reinfections, scientists report in a preliminary study posted May 3 at medRxiv.org (SN:5/27/22). Quach-Thanh has seen an even smaller rate in her own study of health care workers first infected between March and September of 2020. Those data are still unpublished, but she points out that most of the people in her study were vaccinated. “A natural infection with three doses of vaccines protects better than just a natural infection,” she says.
As many families, mine included, gear up for summer camps and vacations, I wanted to learn more about our current COVID-19 risks. I chatted with Quach-Thanh and Anna Durbin, an infectious diseases physician at Johns Hopkins Bloomberg School of Public Health who has studied COVID-19 vaccines. Our conversations have been edited for length and clarity.
What’s the latest on reinfections? Is the picture changing?
Durbin: We have to remember that the virus strain that’s circulating now is very different from the earlier strains. Whether you’ve been infected with COVID-19 or vaccinated, your body makes an immune response to fight future infections. It recognizes [the strain] your body originally saw. But as the virus changes, as it did with omicron, it becomes sort of a fuzzier picture for the immune system. It’s not recognizing the virus as well, and that’s why we’re seeing reinfections.
I’ll also say that reinfections — particularly with respiratory viruses — are very common.
How can scientists distinguish a true reinfection from a relapse of an original infection?
Quach-Thanh: There are multiple ways of looking at this. The first is looking at the time elapsed between the first infection and a new positive PCR test. If it has been more than three months, it is unlikely to be just a remnant of a previous infection. We can also look at viral load. A really high viral load usually means it’s a new infection. But the best way to tell is to sequence the virus [to determine its genetic makeup] to see if it is actually a new strain.
What do we know about the health risks of reinfection?
Quach-Thanh: The good thing is that most of the people who got reinfected [in the Quebec study] got a mild disease, and the risk of hospitalization and death was much lower.
When you get reinfected, you might [have symptoms] like a cold, or even sometimes a cough, and a little bit of a fever, but you usually don’t progress to complications as much as you would with your first infection — if you’re vaccinated.
Does reinfection increase your chance of developing long COVID?
Durbin: I think that’s unknown, but it’s being studied.
As we look back at the omicron wave in the U.S. that happened in January and February, now is about the time we would start to see symptoms of long COVID. So far it looks promising. We seem to be seeing a lower incidence of long COVID [after reinfection with omicron] than we did with primary infection, but those data are going to continue to be collected over the next few months.
At this point in the pandemic, how cautious do we need to be?
Quach-Thanh: It depends on your baseline risk of complications. If you’re healthy, if you’re doing most activities outdoors, if you’re vaccinated, life can proceed. But if you’re immune suppressed or elderly, the situation might be different.
See all our coverage of the coronavirus outbreak
If you have symptoms, it would be advisable to not mingle in indoor settings without a mask so that you don’t contaminate other people. There are immunocompromised people who might be at risk of serious infection. We still need to keep them in mind. I think we have to be responsible, and if we’re sick, we should get tested.
Durbin: This is what I tell my friends, family and patients: This virus is here to stay. Any time you’re in a crowded place with poor ventilation and lots of people, there’s a chance there’s going to be transmission. The risk is never going to be zero. It’s a message people don’t want to hear. But as long as there are people to infect, this virus is not going away.
We have to move to acceptance, and we have to be better members of society. If we can, we should stay home when we’re sick. If we can’t stay home, we should wear a mask. We should wash our hands regularly. These are things that work to reduce transmission.
They reduce your risk of getting not just COVID-19, but also a cold or the flu.
Can we anticipate another surge in cases?
Quach-Thanh: I think the next wave will come in the fall. The problem with this virus is that it mutates. And as long as it’s transmitted, it will continue to mutate.
What can we look forward to?
Durbin: I think young kids getting vaccinated is going to reduce the ability of the virus to spread (SN: 6/17/22). That’s good news.
 A new treatment could restore some mobility in people paralyzed by strokes
A new treatment could restore some mobility in people paralyzed by strokes 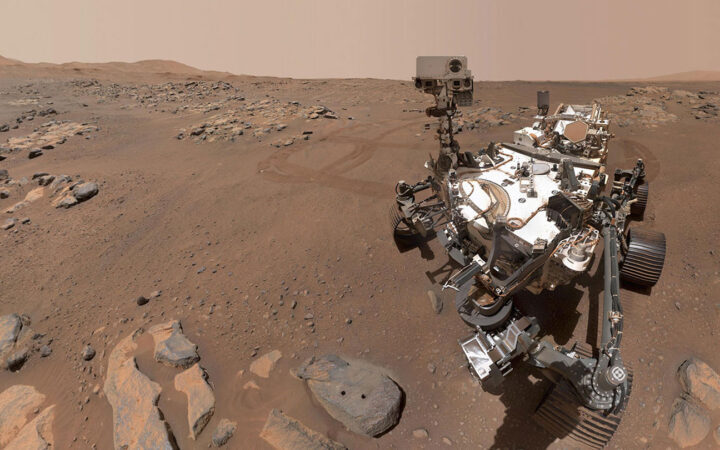 What has Perseverance found in two years on Mars?
What has Perseverance found in two years on Mars? 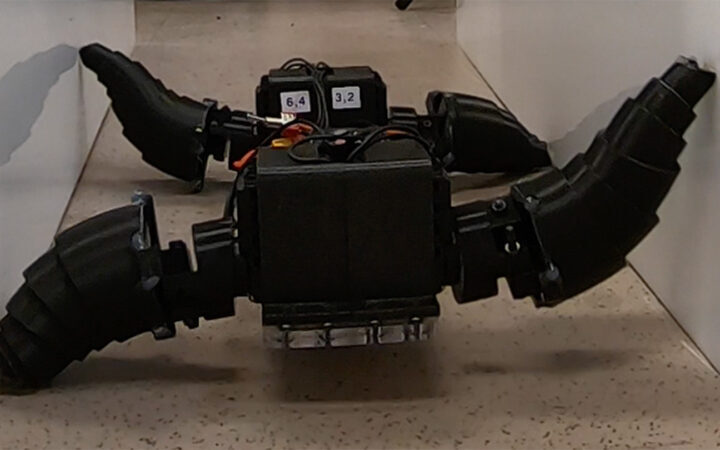 This robot automatically tucks its limbs to squeeze through spaces
This robot automatically tucks its limbs to squeeze through spaces  Greta Thunberg’s new book urges the world to take climate action now
Greta Thunberg’s new book urges the world to take climate action now  Glassy eyes may help young crustaceans hide from predators in plain sight
Glassy eyes may help young crustaceans hide from predators in plain sight 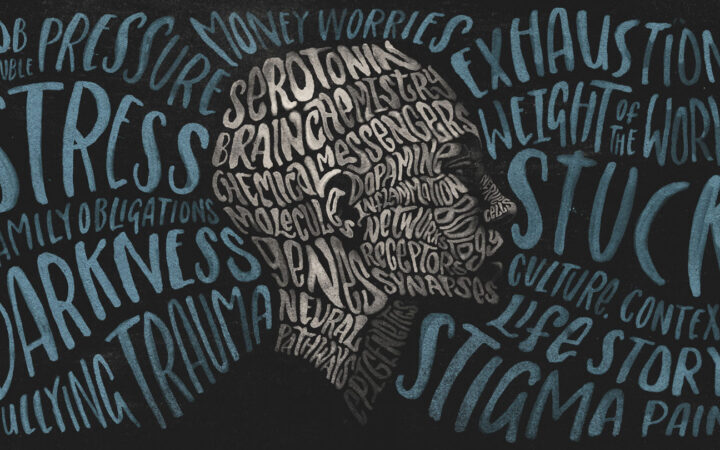 A chemical imbalance doesn’t explain depression. So what does?
A chemical imbalance doesn’t explain depression. So what does?