
A particular kind of poliovirus is spreading in the United States. The U.S. Centers for Disease Control and Prevention has confirmed that the country now joins a list of around 30 other countries where circulation of the virus has been identified. Those countries include the United Kingdom, Israel, Egypt, Yemen and around two dozen in Africa.
The news, announced September 13, comes after the identification in July of a case of paralytic polio in an unvaccinated adult in Rockland County in New York. Public health officials found the case was caused by what’s called a vaccine-derived poliovirus (find out more about this kind of poliovirus below). This spurred wastewater surveillance in Rockland and the surrounding counties, because people shed poliovirus in their stool. The wastewater samples showed that the virus was spreading in Rockland and neighboring areas.
In response, New York Governor Kathy Hochul declared a state of emergency on September 9 to expand access to polio vaccination statewide. Three of the counties where poliovirus has been detected in wastewater — Rockland, Orange and Sullivan — have polio vaccination rates of only around 60 percent. The virus has also turned up in New York City and Nassau County.
While most people infected with polio don’t have symptoms, some might feel like they have the flu, with fever, fatigue or a sore throat. In rare cases, the virus can cause permanent paralysis, and the disease can turn deadly if that paralysis hits the muscles that control breathing or swallowing. Anyone unvaccinated is at risk of paralytic polio if they get infected.
Widespread vaccination efforts helped eliminate wild polioviruses from the United States in 1979, but public health officials are still working toward eradicating the disease globally (SN: 9/12/19). The new worries about polio in the United States are driven by vaccine-derived versions of the virus spreading in areas with low vaccination.
Here are six things to know about polio right now.
There are two types of polio vaccines. What’s the difference?
Polio vaccines come as a shot, given in the arm or leg, or a liquid given orally. These vaccines provide protection against wild poliovirus and vaccine-derived poliovirus. Both polio vaccines used to be given in the United States, but since 2000, the shot has been the only polio vaccine available in the country (SN: 10/27/21).
The shot is an inactivated vaccine given as part of routine childhood vaccinations in the United States. It is made using poliovirus that has been “killed,” stripped of its ability to cause disease. Kids receive a total of four shots. The inactivated vaccine protects against paralysis.
The oral vaccine, still used in many countries, is an attenuated vaccine, made with live but weakened poliovirus. This vaccine can help prevent wild poliovirus from being passed along further if a vaccinated person drinks water or eats food that has been contaminated with stool containing the pathogen. That means it can prevent the spread of poliovirus in a community while also protecting against paralysis (SN: 1/8/21).
But because these attenuated versions can replicate, the virus can spread from cell to cell and possibly to other people. Which leads us to the next question.
What are vaccine-derived polioviruses?
These viruses are related to the oral vaccine. Since the viruses used in the vaccine can replicate, they can spread but they’re too weakened to cause serious disease. The problem comes when an attenuated virus from the oral vaccine spreads among too many people and regains its ability to cause paralysis, says Adam Lauring, a virologist and infectious diseases physician at the University of Michigan in Ann Arbor. “Because it can replicate, it will evolve.”
In a community with low or no vaccination against polio, such vaccine-derived polioviruses can cause disease.
So why do some countries still use the oral vaccine?
The Global Polio Eradication Initiative, which includes the World Health Organization, CDC, United Nations Children’s Fund and other groups, has been working since 1988 to eradicate polio. The oral vaccine has been a key tool for global efforts to get rid of polio, Lauring says. That’s not only because that vaccine is inexpensive and easy to use in low- and middle-income countries, but also because studies suggest it better protects the gut, the part of the body where the virus grows. The more protected the gut, the better the chances of reducing transmission and stopping an outbreak.
What does it mean that poliovirus is being detected in wastewater?
It’s a sign that poliovirus is spreading among people in those regions.
Paralysis from poliovirus is rare — affecting around 1 out of 200 infected people. So the single paralytic case identified in July in New York was already a hint that there may have been hundreds of other infections. The virus has since been detected in wastewater samples from as early as May. The virus’s continued presence in wastewater suggests people are still getting infected and passing it on to others.
Wastewater surveillance provides information on the extent of a virus’ spread in an area. Here, a CDC scientist prepares a sewage sample for poliovirus detection.Holly Patrick, MS, MPH/CDC
Should unvaccinated people get vaccinated?
Yes. “If you don’t know if you received polio shots, then you should probably get your polio shots,” Lauring says. “If you didn’t [get vaccinated], you should get a polio shot.”
Vaccine-derived polioviruses are largely a problem in communities where not enough people are vaccinated. “That’s one piece of the puzzle of what’s been going on in New York,” Lauring says. Low immunization rates mean vaccine-derived viruses can spread, largely among unvaccinated people, and circulate silently before someone gets sick.
Places that have sanitation issues or struggle with other intestinal diseases are also hot spots for vaccine-derived polioviruses. When there’s not enough immunity to stop poliovirus from circulating, the virus can evolve further.
What about people who got vaccinated as kids?
People who got vaccinated, even decades ago, are likely still protected.
Adults who have a high risk of exposure to the virus are eligible for one lifetime booster shot, according to the CDC. Otherwise, people should make sure they received all the recommended doses.
It’s unknown exactly how durable childhood polio vaccines are at protecting against severe disease in adults. With little polio circulating around the world, it’s a hard question to study, Lauring says. Still, for years there haven’t been any cases of polio in the United States, and we’ve largely had immunity from the inactivated vaccine, he says. “I’m not sounding the alarm bells.”
 A new treatment could restore some mobility in people paralyzed by strokes
A new treatment could restore some mobility in people paralyzed by strokes 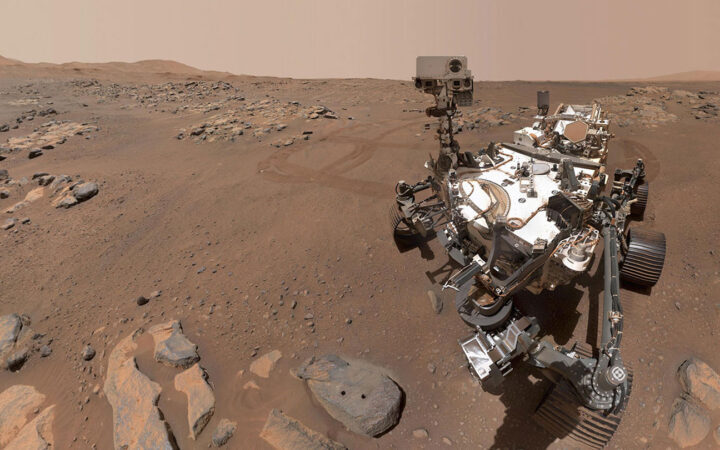 What has Perseverance found in two years on Mars?
What has Perseverance found in two years on Mars? 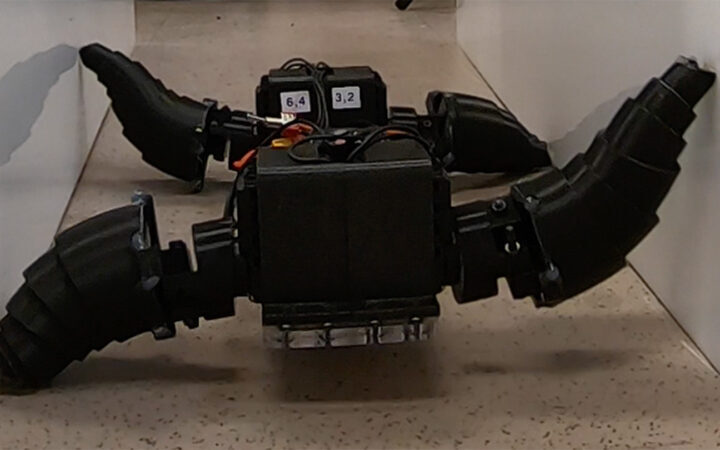 This robot automatically tucks its limbs to squeeze through spaces
This robot automatically tucks its limbs to squeeze through spaces  Greta Thunberg’s new book urges the world to take climate action now
Greta Thunberg’s new book urges the world to take climate action now  Glassy eyes may help young crustaceans hide from predators in plain sight
Glassy eyes may help young crustaceans hide from predators in plain sight 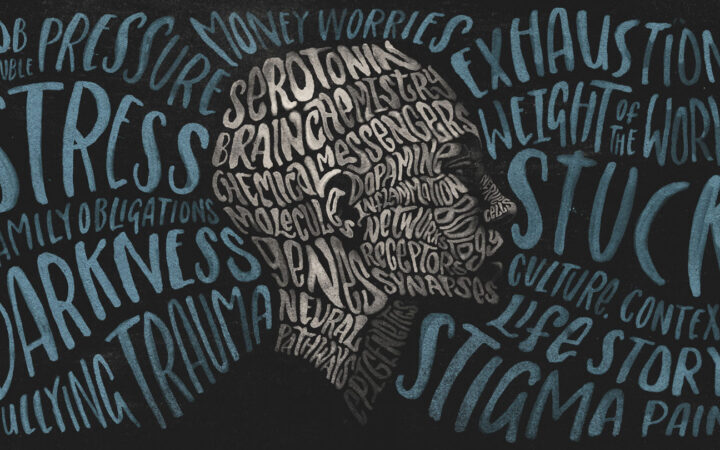 A chemical imbalance doesn’t explain depression. So what does?
A chemical imbalance doesn’t explain depression. So what does?