
A gene-based therapy is potentially a step closer to becoming a one-time treatment for men with hemophilia. The life-threatening genetic disorder hinders the body’s ability to form blood clots.
In hemophilia A, the most common type, the gene responsible for a blood clotting protein called factor VIII has errors, leading the body to produce an insufficient amount of the protein. A new study describes how 132 men with a severe form of the disease who received one infusion of the gene therapy fared. A year later, 88 percent of them had factor VIII levels high enough to have either a mild form or no disease, researchers report March 16 in the New England Journal of Medicine.
Hemophilia A is an inherited disorder. The gene that provides instructions for making factor VIII is found on the X chromosome, so the condition more typically affects males than females. In the United States, there are 12 hemophilia A cases per 100,000 males.
The severity of hemophilia is classified by the amount of factor VIII that the body manages to produce. People with mild disease, who have 5 to 40 percent of typical factor VIII levels, are most likely to have excessive bleeding only after injury or surgery. Moderate hemophilia, with levels 1 to 5 percent of the usual amount, can also include bleeding that occurs spontaneously, without a clear cause. People with severe hemophilia have next to no factor VIII and, without treatment, face frequent, spur-of-the-moment bleeding internally that can damage their joints or brain.
But thanks to the treatment options available, hemophilia patients “now have a normal life expectancy and are encouraged to live normal lives,” says director of the Washington Center for Bleeding Disorders and hematologist Rebecca Kruse-Jarres of the University of Washington in Seattle, who was not involved in the gene therapy study.
The standard treatment to prevent bleeding is a replacement infusion of factor VIII, which is needed every 2 to 3 days. That means a person with hemophilia A could face more than 150 of these treatments a year. More recently, a monoclonal antibody that mimics the action of factor VIII has become available, giving adults and children with the disease a once-weekly treatment option.
The gene therapy, called valoctocogene roxaparvovec, consists of a one-time infusion containing genetic instructions for producing factor VIII, delivered by an adeno-associated virus, which does not cause disease (SN: 10/28/02). The virus is taken up by many different cells, but only liver cells can use the instructions to make the clotting protein.
While most of the study participants saw an improvement in their factor VIII levels, the therapy did not work for a small percentage. And most participants also experienced a concerning side effect — elevated levels of a liver enzyme that can be sign of inflammation or potential damage to the organ, which required treatment with immunosuppressants.
It’s also unclear how long the effects of the treatment will last. The researchers report that in 17 participants followed for two years, the clotting protein levels achieved in the first year decreased in the second year. The gene therapy can only be given once because a person would have an immune response to a second dose. More research is needed to understand the long-term durability of the treatment and the best way to manage the increased liver enzyme levels, says study coauthor and hematologist Margareth Ozelo of the University of Campinas in São Paulo.
“This will be not a treatment for all patients,” Ozelo says, but “will benefit a group of patients in the hemophilia community.” With more work, it may be possible to determine which patients are more likely to respond well to the gene therapy, she says.
Gene therapy could be a wonderful option, because it would almost eliminate the burden of treatments, says Kruse-Jarres. But when considering gene therapy, “a lot of unknowns come into play,” she says.
 A new treatment could restore some mobility in people paralyzed by strokes
A new treatment could restore some mobility in people paralyzed by strokes 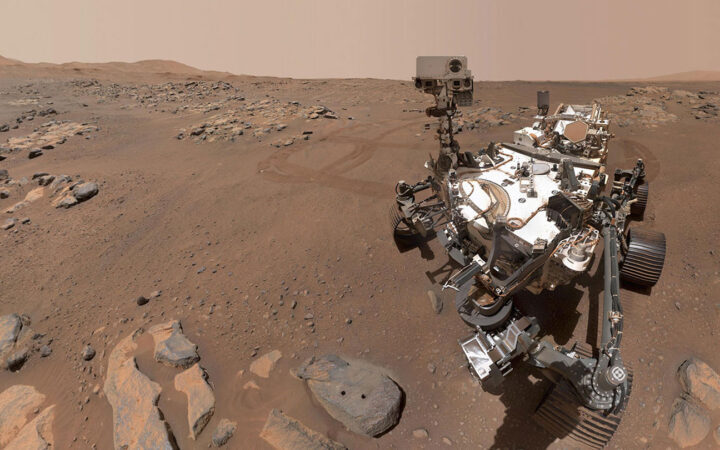 What has Perseverance found in two years on Mars?
What has Perseverance found in two years on Mars? 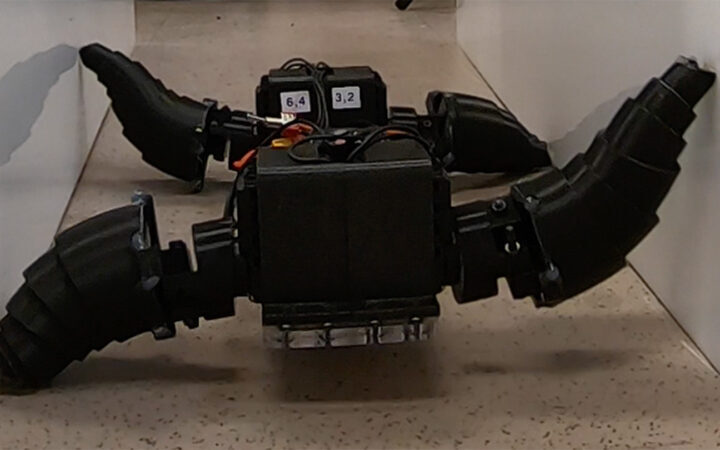 This robot automatically tucks its limbs to squeeze through spaces
This robot automatically tucks its limbs to squeeze through spaces  Greta Thunberg’s new book urges the world to take climate action now
Greta Thunberg’s new book urges the world to take climate action now  Glassy eyes may help young crustaceans hide from predators in plain sight
Glassy eyes may help young crustaceans hide from predators in plain sight 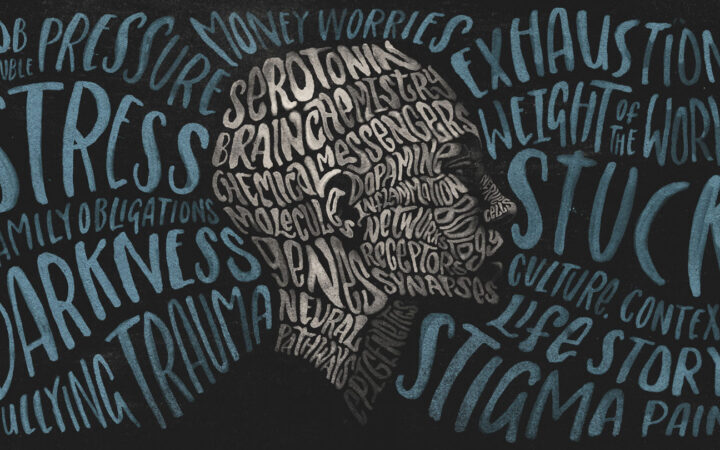 A chemical imbalance doesn’t explain depression. So what does?
A chemical imbalance doesn’t explain depression. So what does?