
A genetic variant that appears to have boosted medieval Europeans’ ability to survive the Black Death centuries ago may contribute — albeit in a small way — to an inflammatory disease afflicting people today.
Researchers used DNA collected from centuries-old remains to discern the fingerprints that bubonic plague during the Black Death left on Europeans’ immune systems. This devastating wave of disease tended to spare those who possessed a variant of a gene known as ERAP2, causing it to become more common, researchers report October 19 in Nature. That variant is already known to scientists for slightly increasing the odds of developing Crohn’s disease, in which errant inflammation harms the digestive system.
The results show “how these studies on ancient DNA can help actually understand diseases even now,” says Mihai Netea, an infectious diseases specialist at Radboud University Medical Center in Nijmegen, Netherlands, who was not involved with the study. “And the trade-off is also very clear.”
Caused by the bacterium Yersinia pestis, bubonic plague once killed 60 percent of those infected (SN: 6/15/22). In the ancient world, it caused successive waves of misery, the most devastating of which was the Black Death, often dated from 1346 to 1350, an episode thought to have wiped out at least 25 million people — about a third or more of the European population.
By sparing individuals whose immune systems bear certain traits, pathogens such as Y. pestis have shaped the evolution of the human immune system. Studies are teasing out the ways the massive winnowing of the plague altered Europeans’ immune-related genetics.
In this most recent study, population geneticist Luis Barreiro of the University of Chicago and colleagues collected samples containing DNA from the remains of 516 people in London and Denmark who died between 1000 and 1800, including those buried during the Black Death. The researchers examined stretches of DNA for immune-related genes and areas associated with autoimmune and inflammatory diseases.
Within those regions, the researchers identified four locations on chromosomes where they saw strong evidence of genetic changes that appeared to have been driven by the Black Death. In follow-up work, one change stood out: an increase in the frequency of a variant of ERAP2. When infected with Y. pestis, immune cells from people with this version of ERAP2 more effectively killed the bacteria than cells lacking the variant. Studies of modern populations have linked that same variant to Crohn’s disease.
While the researchers calculate that the ERAP2 variant improved the odds of surviving the Black Death by as much as 40 percent, it only slightly increases the risk for Crohn’s disease. For complex disorders like Crohn’s, “you require probably hundreds, sometimes thousands of genetic variants to actually increase your risk in a significant manner,” Barreiro says.
For some time now, researchers in the field have theorized that adaptations that helped our ancestors fortify their immune systems against infectious diseases can contribute to excessive, damaging immune activity. Earlier studies of plague offer support for this idea. A genetic analysis seeking traces of historical disease in modern Europeans and a study of DNA from the remains of 16th century German plague victims both turned up what appear to be protective changes against the plague that, like the ERAP2 variant, are linked with inflammatory and autoimmune conditions.
Likewise, this latest discovery suggests that genetic changes that have amped up the human immune response in the past, empowering it to better fight off ancient infections, can come at a cost. “If you turn the heat too much, that leads to disease,” Barreiro says.
 A new treatment could restore some mobility in people paralyzed by strokes
A new treatment could restore some mobility in people paralyzed by strokes 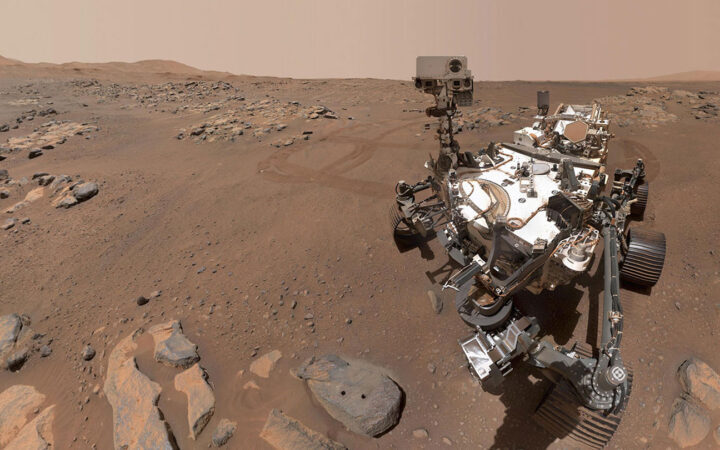 What has Perseverance found in two years on Mars?
What has Perseverance found in two years on Mars? 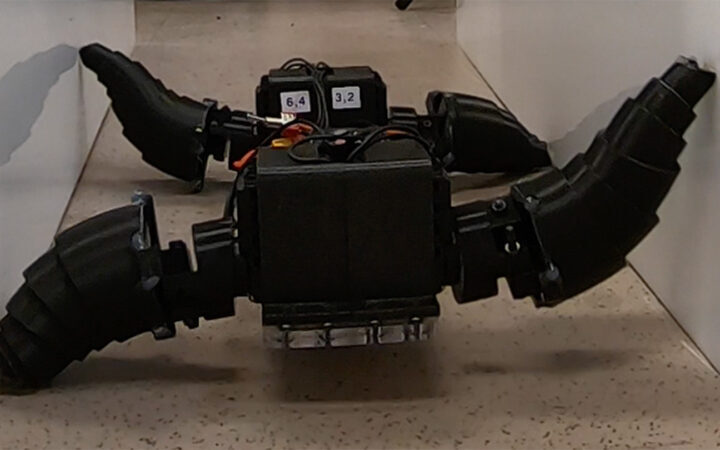 This robot automatically tucks its limbs to squeeze through spaces
This robot automatically tucks its limbs to squeeze through spaces  Greta Thunberg’s new book urges the world to take climate action now
Greta Thunberg’s new book urges the world to take climate action now  Glassy eyes may help young crustaceans hide from predators in plain sight
Glassy eyes may help young crustaceans hide from predators in plain sight 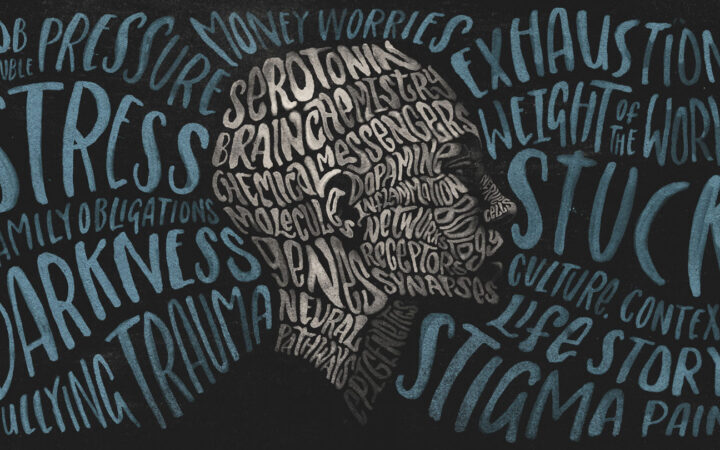 A chemical imbalance doesn’t explain depression. So what does?
A chemical imbalance doesn’t explain depression. So what does?