
As science journalists, we’re accustomed to data. We sift through it and talk it over with experts. We pay close attention to the stories that numbers can tell. But at this point in the pandemic, many of us are having a hard time finding the story. That’s because the numbers aren’t there.
Data on coronavirus infections in the United States have become less reliable, many experts say. Fewer people are getting tested, local governments have stopped reporting results, and home test results rarely make it into official counts (SN: 4/22/22).
Sign up for e-mail updates on the latest coronavirus news and research
To be sure, there are still official numbers to be found. They don’t look great. Hospitalizations are low compared with earlier in the pandemic, but they’re rising again, and the case counts that do exist are ticking up, too. After dipping in March, the tally in the United States is back up to more than 100,000 known cases a day. A third of Americans now live in places with “medium to high” levels of virus spread.
With these not-so-great numbers in mind, it’s not a stretch to assume that the missing data probably wouldn’t tell us a cheery story either. We are almost certainly undercounting cases in the United States. And we’re not alone. Amid worldwide declines in testing and sequencing to see where coronavirus is spreading and how it’s changing, “we are blinding ourselves to the evolution of the virus,” Tedros Adhanom Ghebreyesus, the head of the World Health Organization, said May 22.
We’ve never had a perfect count of COVID-19 cases, of course. Early on in the pandemic, before testing ramped up in some places, scientists found clues about COVID-19’s transmission in odd places. Wastewater testing, for instance, spotted signs of the virus getting flushed down the toilet (SN: 5/28/20). That dirty water continues to be an indirect, but helpful, measure of viral loads in a community. Here in Oregon, where I live, some wastewater spots again show increases in coronavirus, suggesting a surge.
Even more indirect measurements can give us additional hints. Early on in the pandemic, “smart” thermometers connected to the internet generated fever data used to map risk of getting sick by region. Internet searches for words and phrases, such as “chills,” “fever” and “I can’t smell,” also pointed to virus hot spots.
My favorite digital sign of illness comes from online reviews of Yankee Candles. One-star reviews (“No scent.” “Embarrassed as this was a gift.”) tracked neatly with a rise in COVID-19 cases in 2020 and the subsequent loss of smell. Just last week, more one-star reviews showed up, notes Twitter user @drewtoothpaste, who compiled the latest complaints. “No smell.” “Absolutely no scent.” “Very disappointing!!!”
See all our coverage of the coronavirus outbreak
These one-star reviews are not airtight evidence of COVID-19 rates — not by any stretch. But they add to the broader picture that we are not yet done with this pandemic, as much as we would all love to be. We are still experiencing disruptions to our lives, illness, suffering and sadness. Very disappointing indeed.
To better understand this particular moment in the pandemic, I talked with data expert Beth Blauer of Johns Hopkins University. She’s been tracking metrics of the pandemic since it started. In the earliest days, she helped build databases, including a widely used COVID-19 tracker, that ultimately became the Coronavirus Resource Center at Hopkins. Those tools get data out to other scientists, health experts, government leaders, journalists and people who want to keep up with the latest numbers. The interview has been edited for length and clarity.
SN: How solid is the testing data right now in the United States?
Blauer: The testing data in this country is crumbling…. We’re barely getting data out of the application-based resources that come with home tests. And the home tests are running 10 bucks apiece. That’s cost prohibitive for people who live below the poverty line. Even middle-income people are not spending $20 for a pack of two. [Free tests are available in the United States, but it’s not known how many of those tests are reaching people who need them.]
We are flying blind. Completely. We are in a surge right now, but we don’t even appreciate fully how big of a surge this is.
SN: Any guesses?
Blauer: I have no idea. Anecdotally, I’m sure you and I both know a ton of people who have COVID-19 or who just got over it. All the mitigation strategies are not being spun up to meet the rising demand that a surge, like we’re in right now, calls for, which means we’re just going to be getting a lot more COVID-19. People are going on vacations, they’re traveling, graduations, all of these things are just going forward. So yes, we’re seeing some increase in hospitalization, but I don’t think we have any idea how much disease there is in the community.
SN: I’ve had trouble gauging my risk from COVID-19 in everyday life. Is that typical?
Blauer: It’s a mess. I think a lot of people are sensing that. And it dilutes our capacity to have faith in science and in all the things that have happened over time. It is confusing. It’s like, “Oh, we have just as much COVID, but we can go to parties? And school is in?” Everything all of a sudden gets called into question.
[That uncertainty highlights a] need to really think critically about our public health infrastructure in this country.
SN: How should we be living with this virus right now?
Blauer: We all acknowledge that we need social anchoring in our communities. We need to see people. We can’t hide away in our houses forever. But that means we have to think about what it means to live with a pathogen like COVID-19 out there. And we’re not giving ourselves all the best tools to be able to do that.
I work in a building where right down the hall, people are getting chemotherapy. I feel a responsibility to the community that I’m not giving them a disease that could potentially kill them. That’s not happening in a lot of places. For me, it’s sad. It’s like a loss of collective empathy, and I don’t think we should not talk about that.
I think I would feel the very same way even if I wasn’t leading this effort here at Hopkins. But I don’t know. Maybe it’s because I feel the toll of a million Americans who have died. I’ve experienced loss in my life. I do have a lot of empathy. But I don’t think I’m overdoing it.
SN: But you’re not saying we should all hunker down and stay away from people.
Blauer: No. We’re done with that. But we have to start integrating and really putting into place these habits [masking, testing and adjusting behavior when needed]. Because I think it’s the only way we get out of this.
 A new treatment could restore some mobility in people paralyzed by strokes
A new treatment could restore some mobility in people paralyzed by strokes 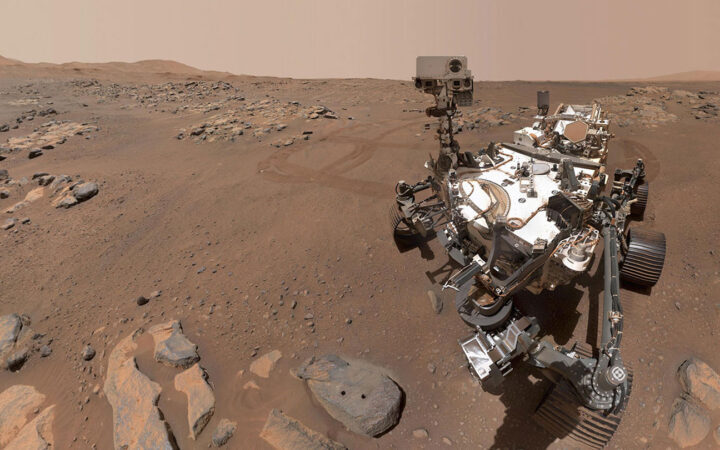 What has Perseverance found in two years on Mars?
What has Perseverance found in two years on Mars? 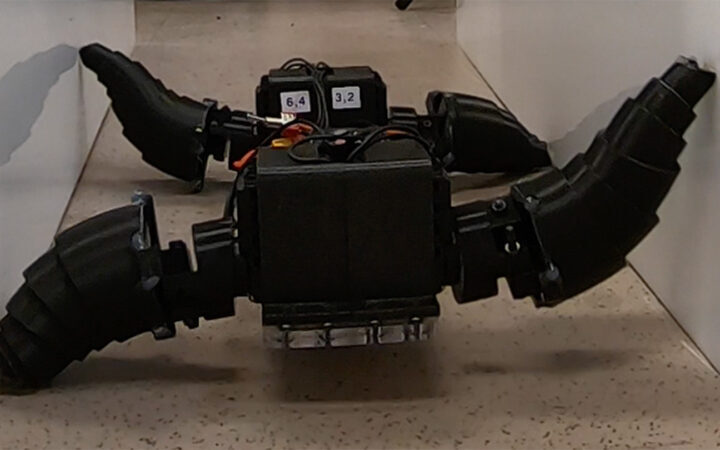 This robot automatically tucks its limbs to squeeze through spaces
This robot automatically tucks its limbs to squeeze through spaces  Greta Thunberg’s new book urges the world to take climate action now
Greta Thunberg’s new book urges the world to take climate action now  Glassy eyes may help young crustaceans hide from predators in plain sight
Glassy eyes may help young crustaceans hide from predators in plain sight 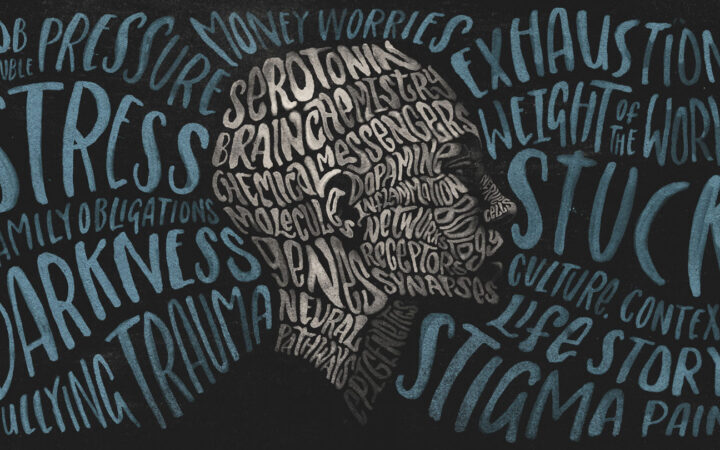 A chemical imbalance doesn’t explain depression. So what does?
A chemical imbalance doesn’t explain depression. So what does?