
You may have heard the big long COVID news that came out recently: A Scottish study reported that about half of people infected with SARS-CoV-2 have not fully recovered six to 18 months after infection. That result echoes what many doctors and patients have been saying for months. Long COVID is a serious problem and a huge number of people are dealing with it.
But it’s tough to find treatments for a disease that is still so ill-defined (SN: 7/29/22). One major research effort in the United States hopes to change that. And one of my colleagues, Science News’ News Director Macon Morehouse, got a peek into the process.
In the last two months, Morehouse has donated 15 vials of blood, two urine specimens and a sample of saliva. Technicians have measured her blood pressure, oxygen level, height, weight and waist circumference and counted how many times she could rise from sitting to standing in 30 seconds. Morehouse is not sick, nor is she collecting data for her health. She’s doing it for science.
Morehouse is participating in a long COVID study at Howard University in Washington D.C. It’s part of a many-armed giant of a project with an eye on one thing: the long-term health effects of COVID-19. Launched last year by the National Institutes of Health, the RECOVER Initiative aims to enroll roughly 60,000 adults and children. At the Howard site, Morehouse is volunteer No. 182.
She’s somewhat of a unicorn among study participants: As far as she knows, Morehouse has never had COVID-19. Ultimately, some 10 percent of participants will include people who have avoided the virus, says Stuart Katz, a cardiologist and a RECOVER study leader at NYU Langone Health in New York City. Scientists continue to sign up volunteers, but “omicron made it harder to find uninfected people,” he says.
RECOVER scientists need participants like Morehouse so the researchers can compare them with people who developed long COVID. That might reveal what the disease is — and who it tends to strike. “Our goals are to define long COVID and to understand what’s your risk of getting [it] after COVID infection,” Katz says. Their results could be a first step toward developing treatments.
Tight timeline
Within the pandemic’s first year, doctors noticed that some COVID-19 patients developed long-term symptoms such as brain fog, fatigue and chronic cough. In December 2020, Katz and other physicians and scientists convened to discuss what was known. The answer, it turned out, was not much. “This is a novel virus,” he says. “Nobody knew what it could do.” Around the same time, Congress OK’d $1.15 billion for the NIH to study COVID-19’s long-term health consequences.
Fast forward five months, and the agency had awarded nearly $470 million to NYU Langone Health to serve as the hub for its long COVID studies. “The whole thing was on a very, very compressed timeline,” Katz says. NYU then hustled to come up with a study plan focused on three main groups: adults, children/families and finally, tissue samples from people who died after having COVID-19. It wasn’t your typical research project, Katz says. “We were charged with studying a disease that didn’t have a definition.”
Today, RECOVER has enrolled just over half of a target 17,680 adults. Katz hopes to cross this finish line by spring 2023. The child-focused part of the project has further to go. The goal is to enroll nearly 20,000 children; so far, they’ve got around 1,200, says Diana Bianchi, director of the Eunice Kennedy Shriver National Institute of Child Health and Human Development and a member of RECOVER’s executive committee.
Sign up for e-mail updates on the latest coronavirus news and research
Some scientists and patients have criticized RECOVER for moving too slowly. As someone who has recovered from long COVID himself, Katz says he gets it. “We started a year and a half ago, and we don’t yet have definitive answers,” he says. “For people that have been suffering, I can understand how it’s disappointing.”
But for RECOVER — with more than 400 doctors, scientists and other experts involved, roughly 180 sites across the country enrolling participants and a grant timeline that scuttled the usual order of events — the old saying about building the plane while flying it fits, Katz says. “We are working very, very hard to move as quickly as we can.”
Looking for answers
Recently, other facets of the initiative have started to shine. An analysis of electronic health records found that among people under 21, kids younger than 5, kids with certain medical conditions and those who had had severe COVID-19 infections may be most at risk for long COVID, scientists reported in JAMA Pediatrics in August. And a different health records study suggests that vaccinated adults have some protection against long COVID, even if they had a breakthrough infection. Scientists posted that finding this month at medRxiv.org in a study that has yet to be peer-reviewed.
These studies tap data that have already been collected. The bulk of the RECOVER studies will take longer, because scientists will follow patients for years, analyzing data along the way. “These are observational, longitudinal studies,” Katz says. “There’s no intervention; we’re basically just trying to understand what long COVID is.”
Still, Katz expects to see early results later this fall. By then, scientists should have an official, if rough, definition of long COVID, which could help doctors struggling to diagnose the disease. By the end of the year, Katz says RECOVER might also have answers about viral persistence — whether coronavirus relics left behind in the body somehow reboot symptoms.
The project has also recently sprouted a clinical trials arm, which may launch this winter, says Kanecia Zimmerman, a pediatric critical care specialist who is leading this effort at the Duke Clinical Research Institute in North Carolina. One of the first trials planned will test whether an antiviral therapy that clears SARS-CoV-2 from the body helps patients with persistent symptoms.
Though RECOVER is a major effort to understand long COVID, progress will require research — and ideas — from a broad group of scientists, says Diane Griffin, a microbiologist at the Johns Hopkins Bloomberg School of Public Health in Baltimore and member of the Long COVID Research Initiative, who is not involved in the project. “Just because we’ve invested in this one big study, that’s not going to give us all the answers,” she says.
But information from study participants like Morehouse and the nearly 10,000 other adults who’ve already enrolled in RECOVER will help. In the meantime, continued support for long COVID research is crucial, Griffin says. “That’s the only way we’re going to eventually figure this out.”
 A new treatment could restore some mobility in people paralyzed by strokes
A new treatment could restore some mobility in people paralyzed by strokes 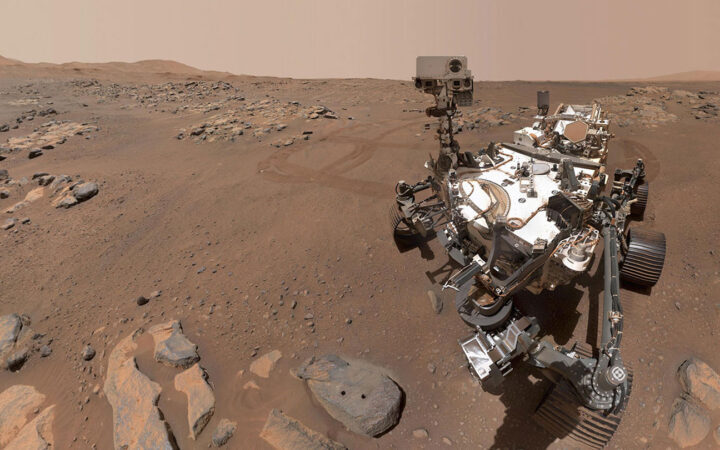 What has Perseverance found in two years on Mars?
What has Perseverance found in two years on Mars? 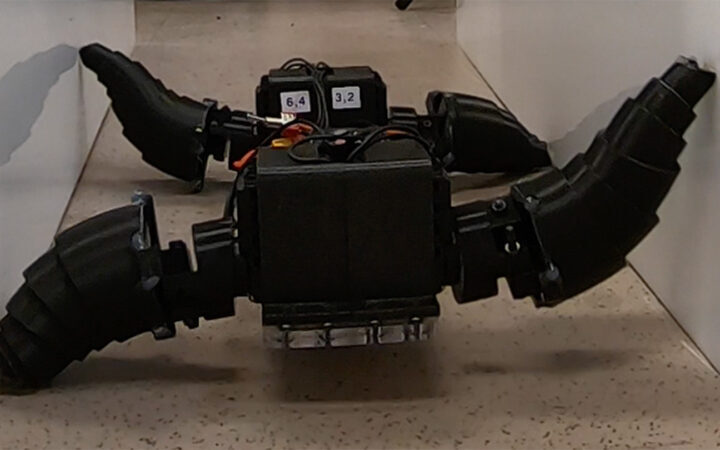 This robot automatically tucks its limbs to squeeze through spaces
This robot automatically tucks its limbs to squeeze through spaces  Greta Thunberg’s new book urges the world to take climate action now
Greta Thunberg’s new book urges the world to take climate action now  Glassy eyes may help young crustaceans hide from predators in plain sight
Glassy eyes may help young crustaceans hide from predators in plain sight 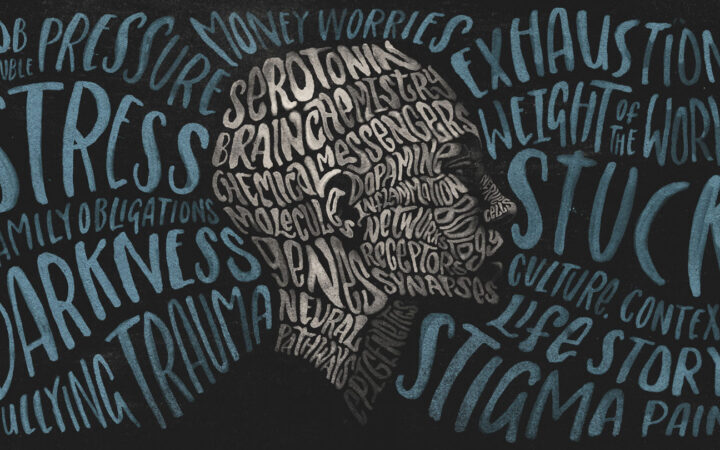 A chemical imbalance doesn’t explain depression. So what does?
A chemical imbalance doesn’t explain depression. So what does?