
In early 2022, malaria cases in the Ethiopian city of Dire Dawa surged, with more than 2,400 people sickened. The spike in infections was the work of an invasive mosquito species that’s spreading across Africa, scientists report.
The finding, presented November 1 in Seattle at the annual meeting of the American Society of Tropical Medicine and Hygiene, provides evidence that the invasive vector can drive malarial outbreaks. Worryingly, the species can thrive in urban environments, bringing the threat of malaria to potentially many millions more people across the continent.
Anopheles stephensi is a mosquito native to India and the Persian Gulf, where it is a major vector for the Plasmodium parasites that cause malaria in people (SN: 10/26/20). In Africa, the primary malaria vector is Anopheles gambiae. A. stephensi was first reported on the African continent in Djibouti in 2012. Since then, the species has turned up in other African countries such as Ethiopia, Somalia and Nigeria.
It wasn’t clear what kind of malarial burden the invasive mosquito could bring to Africa, says Fitsum Girma Tadesse, a molecular biologist at the Armauer Hansen Research Institute in Addis Ababa, Ethiopia. In the eight years after the mosquito’s arrival in Djibouti, the country reported a 40-fold increase in yearly malaria cases, Tadesse says. But no one had directly linked A. stephensi to the increase.
So when malaria cases suddenly rose in Dire Dawa — from 27 cases to 260 in just three weeks in early 2022 — Tadesse and his team jumped in to investigate.
The researchers tracked 80 patients in the city who had sought care for malaria at a local or university clinic, as well as 210 patients who had sought treatment for other reasons, and they screened the patients’ household members for malaria. The team also scanned the patients’ neighborhoods for the presence of mosquito adults and larvae within a 100-meter radius of households, or in the cases of students that visited a clinic, dormitories.
The team found that the malaria patients primarily lived near water sources used by the invasive mosquito, A. stephensi. Households and dorms close to aquatic habitats harboring A. stephensi larvae were 3.4 times as likely as those not close to such water sources to have a family or dorm member test positive for malaria. And most of the adult mosquitoes the team caught — 97 percent — were of the invasive species, the only mosquito species that the researchers found carrying Plasmodium parasites.
A. stephensi “prefers to breed in water storage containers that are typically common in rapidly expanding urban settings,” Tadesse says. The native mosquito species, A. gambiae, tends to use natural sources of water like small pools, which are more common in rural regions, he adds. The concern, then, is that with the expansion of A. stephensi alongside urbanization in Africa, the mosquito could exploit many new sources of water stores.
“This expands the malaria problem from a predominantly rural problem to an urban problem,” says Teun Bousema, an epidemiologist at Radboud University in Nijmegen, the Netherlands.
A 2020 study from another research group estimated that if the invasive mosquito were to spread widely on the continent, an additional 126 million people in cities could be at risk of contracting malaria.
“The spread of Anopheles stephensi is concerning because this species has a number of characteristics that make it difficult to control,” says Tanya Russell, a medical entomologist at James Cook University in Townsville, Australia, who was not involved in the study. Not only can the insects lay their eggs in nearly any available water source, but also the eggs can survive being dry for long periods of time. “This is very uncharacteristic for malaria vectors.”
Insecticide-treated bed nets and spraying a residual insecticide indoors are the primary vector control approaches for malaria-carrying mosquitoes, Russell says. But since A. stephensi also bites outdoors, the mosquito’s spread may blunt the efficacy of these tools.
The key next steps, Tadesse says, are interventions to reduce transmission of the deadly parasites, including targeting the mosquito’s larval phase with chemicals and encouraging communities to cover and secure water containers to prevent mosquitoes from laying eggs in them.
“The window of opportunity to do something about this species is closing,” Bousema says. “So, I really think this calls for very urgent action.”
 A new treatment could restore some mobility in people paralyzed by strokes
A new treatment could restore some mobility in people paralyzed by strokes 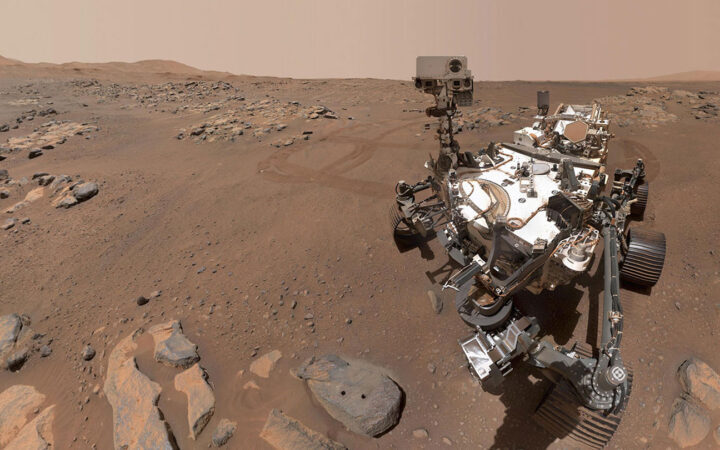 What has Perseverance found in two years on Mars?
What has Perseverance found in two years on Mars? 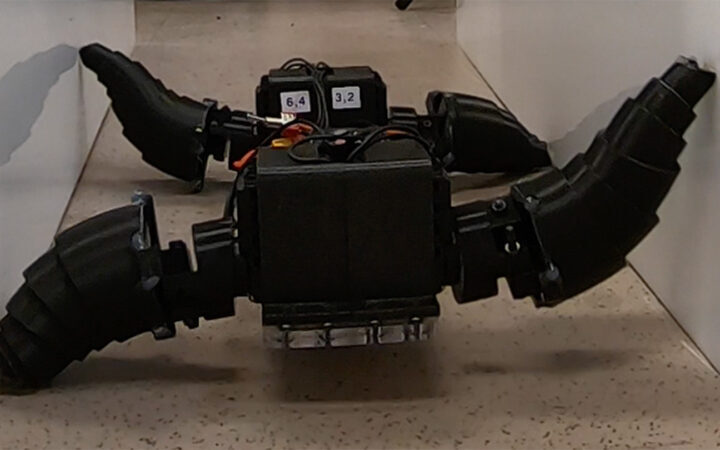 This robot automatically tucks its limbs to squeeze through spaces
This robot automatically tucks its limbs to squeeze through spaces  Greta Thunberg’s new book urges the world to take climate action now
Greta Thunberg’s new book urges the world to take climate action now  Glassy eyes may help young crustaceans hide from predators in plain sight
Glassy eyes may help young crustaceans hide from predators in plain sight 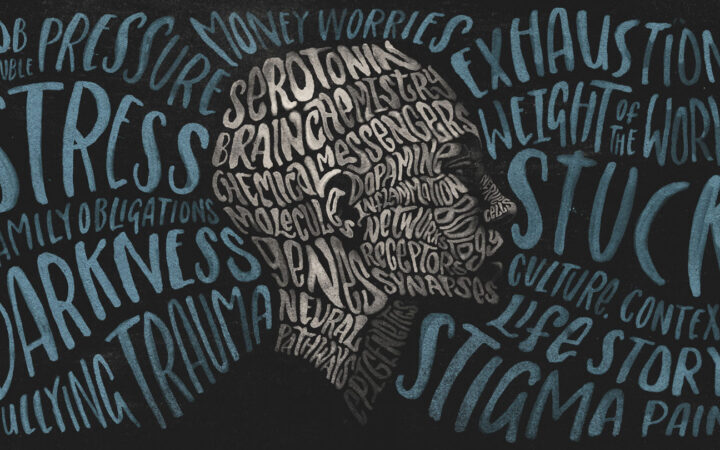 A chemical imbalance doesn’t explain depression. So what does?
A chemical imbalance doesn’t explain depression. So what does?