
One year ago, the World Health Organization declared that the novel coronavirus outbreak was a pandemic (SN: 3/11/20). Little did we know the uncertainty, anxiety, frustration and loss that was in store. It’s been a year that’s felt never-ending. It’s tested us all. It’s cost millions of lives, even as we’ve made remarkably rapid strides in understanding this new foe and finding ways to fight it.
Now, as more and more people get vaccinated against COVID-19, there’s hope that the end of the pandemic is in sight.
We asked five scientists who are among the many who have jumped in to tackle the coronavirus what has surprised them about the past year and what they’ve learned that could help us all as we enter the second year of the pandemic. Their answers have been edited for brevity and clarity.
What has surprised you over the past year?
Rajesh Gandhi, an infectious diseases physician at Massachusetts General Hospital and Harvard Medical School in Boston: What really hits home is that we were not prepared, despite concerns that have been raised for many years that this was coming. We had to essentially prepare and implement our response to the pandemic during the pandemic, as opposed to before.
Damir Huremovic, a psychiatrist with Northwell Health in Manhasset, N.Y.: We constantly keep doing the wrong things; we can’t get our act together. That is probably because of some of the features of this virus. It’s sitting on the border of very dangerous and not so dangerous. It’s playing tricks on our abilities to approximate risk.
I’m angry at myself for failing to foresee that the misinformation that we described in our book [The Psychiatry of Pandemics] in the chapter on immunizations is really not limited to vaccines. It’s more universal … So many people believe that this pandemic is all a hoax. As delusional as [that belief] may be from a psychiatric perspective, we still have to deal with it as a real issue. I wish I had become aware of this phenomenon much sooner.
Maimuna Majumder, a computational epidemiologist at Boston’s Children’s Hospital and Harvard Medical who uses data from search trends, social media and local news to simulate the trajectory of outbreaks: There’s still plenty left to unearth about COVID-19, but I think it’s fair to say that the speed of the research done to date – with the goal of saving lives in mind – has been record-breaking.
Kimberly Prather, an atmospheric chemist and aerosol scientist at the University of California, San Diego and Scripps Institute of Oceanography who urged the World Health Organization and the U.S. Centers for Disease Control and Prevention to say that the coronavirus spreads through the air (SN: 7/7/20): The pushback over acknowledging that this virus is in the air, is airborne … [from] public health agencies and others. I cannot believe the resistance because all the evidence suggests that it’s there. … If we acknowledge that it’s in the air, we can fix it. There’s so many fixable solutions to the problem. It’s killing me.
Jonna Mazet, an epidemiologist and founding executive director of the UC Davis One Health Institute, which focuses on the interplay between the health of animals, people and the environment: The politicizing of health and the resulting separation and divisions. That resulted in people making really different and sometimes risky choices for their own health. I did not anticipate that issue.
On the science side … the way scientists are raised in science is to be successful, publish and be noticed. I think people rallied to the greater global good and put that down and worked together across all kinds of boundaries. Geographic, disciplinary, and [across sectors] like academic, government, private sector — so that was a beautiful surprise. We should all hope we can continue it.
What have you learned that is going to help us navigate the second year of the pandemic?
Prather: The most important thing we can do is help the public understand that [coronavirus is] in the air. We need to ventilate, add filtration, wear masks. I just really believe that the public has been easily confused by all the messaging. In Year 2, if we can just get the message out there that it is in the air. It’s more important to clean the air than it is for surfaces.
Just saying “ventilation” and “filtration” as we have been doing isn’t quite enough. We have to provide better metrics for people to use to know that their businesses or whatever are safe for people to be in.
Majumder: [Having] multiple vaccines work at preventing serious illness is a major win that will help us better navigate the next year.
Gandhi: Doing clinical trials is not only possible during a pandemic, it’s absolutely necessary. You can’t make any progress on treatment unless you do trials during a pandemic. Otherwise you have no idea what works and what doesn’t work, and that’s what March [2020] was like.
Even though the progress has not been as fast as anyone would have liked, we now have several drugs that we have strong evidence for. [That] only came because of imperative clinical trials. So that was a big lesson that I think we knew from medicine but it was never more forcefully demonstrated than in a pandemic.
Huremovic: It’s very simple. We really need to redefine epidemiology as, at least in part, behavioral science. Of course, we can’t disregard the replication of the virus. But we also need to focus on the human behaviors, attitudes, values and reasoning driving this pandemic. The virus is basically just looking to replicate. We are the ones providing the pathways for the virus to replicate.
COVID-19 is the warning shot. This is not the worst that can happen to us. We can take what we have learned about human behavior and how we think in situations like this so that we can help curb an outbreak next time.
Mazet: We can come together and address big problems that are not necessarily the one problem du jour. Right now, we obviously all want, need desperately to get this pandemic under control. But if we really look at the drivers for the pandemic, we can see that they are also drivers for things like climate change. And those climate change factors are also accelerating our risk of being exposed to emerging viruses — things like population growth, the way we use land, the way that we travel and impact the Earth.
All of those things put us into a situation where pathogens can spread rapidly. But climate change, for example, changes the distribution of the potential hosts for viruses and brings them to human populations that wouldn’t have been exposed, historically. These things are all [raising our] risk for negative consequences of life on Earth.





 A new treatment could restore some mobility in people paralyzed by strokes
A new treatment could restore some mobility in people paralyzed by strokes 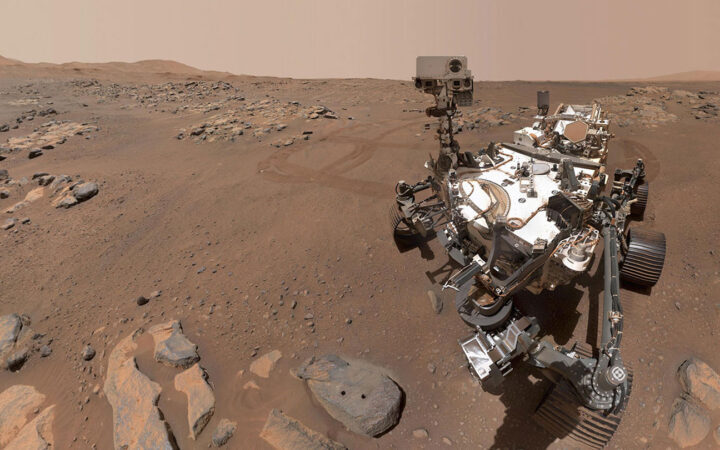 What has Perseverance found in two years on Mars?
What has Perseverance found in two years on Mars? 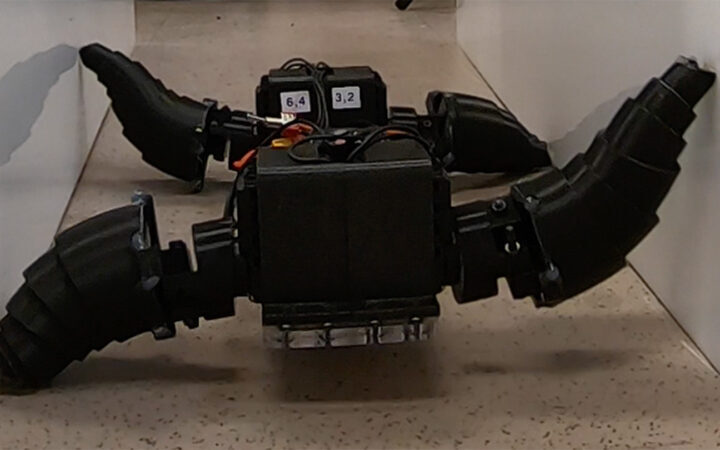 This robot automatically tucks its limbs to squeeze through spaces
This robot automatically tucks its limbs to squeeze through spaces  Greta Thunberg’s new book urges the world to take climate action now
Greta Thunberg’s new book urges the world to take climate action now  Glassy eyes may help young crustaceans hide from predators in plain sight
Glassy eyes may help young crustaceans hide from predators in plain sight 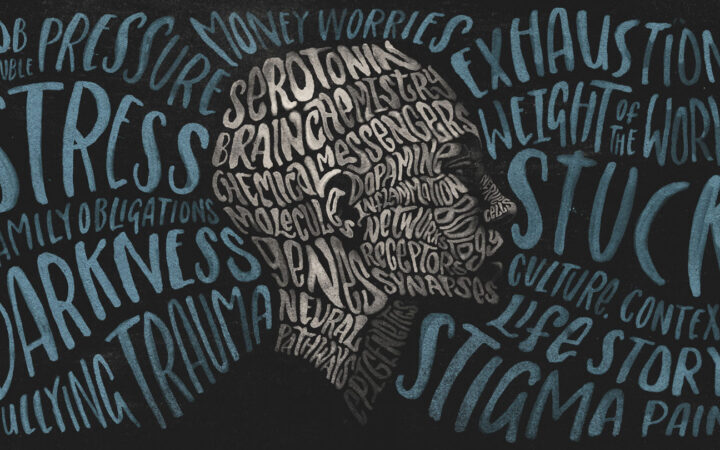 A chemical imbalance doesn’t explain depression. So what does?
A chemical imbalance doesn’t explain depression. So what does?