I’m one of 40 percent or fewer of Americans who have managed to avoid getting COVID-19. I have been avoiding it like a potentially life-threatening virus — I’d say the plague, but all I really do to avoid that illness is not interact with rodents when I visit the West and Southwest. To protect against COVID-19, I wear KN95 masks when I’m indoors in public or in crowded outdoor situations. I’m up-to-date on vaccines with my second booster shot as of May, which may provide a tiny bit of protection against infection, but is mostly for keeping me from getting really sick if I were to get infected (SN: 4/29/22).
And yet, I recently invited COVID-19 into my home. It came in the form of a relative who tested positive while vacationing here. She isolated herself in her hotel room until it was time to check out, but needed a place to stay until she was safe to fly home, according to this quarantine and isolation calculator from the U.S. Centers for Disease Control and Prevention.
She was still testing positive for SARS-CoV-2, the virus that causes COVID-19, on at-home antigen tests when she came to us, so we assumed she was contagious to me and my husband. I made that assumption based on research and conversations with experts. A recent study in the New England Journal of Medicine found that people infected with the omicron variant BA.1 produced infectious virus for about six to eight days on average, with some people shedding infectious virus for 10 days or longer.
We didn’t know which of the omicron variants now circulating my relative had, but we did know that we didn’t want to catch it. Omicron carries a higher chance of being passed on to household members than earlier variants of concern did, a recent JAMA Network Open study found. For instance, omicron had a secondary household attack rate of 42.7 percent, referring to the percentage of household members who got COVID-19 from an infected person in the house. That beats other highly infectious variants by a mile: Alpha’s rate was 36.4 percent and delta’s 29.7 percent. And the currently circulating subvariant of omicron, BA.5, may even reinfect people who recently had COVID-19 (SN: 6/27/22).
So how do you evade a virus that has been catching up with even those who have so far managed to avoid infection for years? A lot of people are probably asking that question right now, given that the CDC’s community transmission map is red across the country (more than 93 percent of counties are reporting high community transmission), and my own personal gauge — Anna Gibbs’ reporting on experts’ advice on what to do after a positive COVID test — is consistently among Science News’ most-read stories (SN: 4/22/22).
Sign up for e-mail updates on the latest coronavirus news and research
“There’s a bunch of different options, and you could do one or many of them, depending on your situation and how concerned you are about getting it,” says Linsey Marr, an aerosol scientist who studies disease transmission at Virginia Tech in Blacksburg.
The first option is to isolate the infected person from the rest of the household. For most people that probably involves putting someone in a room alone and closing the door. We did an admittedly extreme version of secluding our COVID-19 patient by putting up plastic sheeting to wall off our guest bedroom and guest bathroom as an isolation suite. Making things as airtight as possible may help limit the virus’ spread in the house, Marr says. You don’t need to erect a plastic wall like we did, though. Rolling up a towel and sticking it under the door may reduce the amount of air flowing in and out of an infected person’s room. That is a tactic Marr says she uses when staying in hotel rooms.
In our house, my relative went into the isolation suite and emerged only to retrieve meals I left for her on a tray just outside the zipper and to go for brief (masked) walks around the neighborhood.
But not everyone has such a high tolerance for solitude or has a housing situation that allows for a sick ward. And it’s not really feasible to isolate children or household members that need care. Our isolation suite wouldn’t have worked for Marr’s 14-year-old son, she says. “He’s very social. It would have been torture to make him stay in his room.”
Not to worry. Marr says there are plenty of ways to keep the virus away from uninfected family members. Good quality face coverings, such as N95, KN95 or KF94 masks, can help keep the virus in check (SN: 3/25/22). “The most important person to have wear a mask is the infected person because it acts as source control to keep the virus from getting out in the air,” Marr says. Uninfected family members can wear masks as an extra layer of protection, too. My relative graciously wore her mask when outside of the isolation suite, and my husband and I masked and gloved up when we dropped off meals and retrieved dishes.
But Marr’s son wasn’t keen on wearing a mask, so her family took other measures. “We had a portable air cleaner and moved that around with him wherever he was. We did eat dinner together. We opened a window and had him sitting closest to the window with a fan pointing out, so that everything from him was getting sucked out.” Their plan worked. Nobody else in Marr’s household got COVID-19.
“Increased ventilation, of course, is going to be very helpful,” she says. That might involve opening windows when the weather allows and running the bathroom and kitchen exhaust fans. Pointing a fan out the open window in an infected person’s room will also help limit the amount of virus reaching the rest of the household. Open windows aren’t always welcome, especially when it’s too cold or hot outside or during allergy season or when other conditions degrade air quality. For instance, “this assumes your outdoor air is not full of wildfire smoke,” Marr says.
Filtering the air can also reduce the amount of virus floating around the house. We put a portable air cleaner in the isolation suite. And we built a Corsi-Rosenthal box to filter any stray virus that wandered into our air space. The box is a do-it-yourself alternative to pricey HEPA filters. We built ours from four large air filters, a box fan and the cardboard box the fan came in (for the bottom of the box and a shroud for the top). Such boxes aren’t HEPA filters, but they have a higher clean air delivery rate than many commercial machines because they move so much air, Marr says. Still, the box wasn’t cheap to build. It cost about $130, with each filter costing just under $25.
A Corsi-Rosenthal box, built with a box fan and air filters can suck the coronavirus, allergens and irritants out of the air. This is the one we built to filter out SARS-CoV-2 when an infected relative visited.T.H. Saey
“All of these things you can do will reduce your risk by some amount, and the more you layer on top of each other, the more you reduce your risk,” Marr says. Also important is to keep vulnerable people away from the infected person. Vulnerable people include the elderly, immunocompromised people or others with medical conditions that put them at high risk of severe disease.
The good news is that once the infection is over, the virus is probably gone. “The air doesn’t typically stick around in a house, even when everything is closed up … for more than a few hours. It leaks in and out,” Marr says. As for cleaning surfaces and laundry, there’s no need to buy special products. “Regular soap will easily kill the virus,” she says.
Our relative’s positive line on at-home antigen tests grew fainter and fainter and finally disappeared during her stay. Now, more than a week after her departure, my husband and I are still feeling fine and getting negative results on our at-home tests. It wasn’t easy and it certainly wasn’t fun (especially for my sequestered relative) to ward off the pestilence within our walls, but it’s possible. If the coronavirus invades your home, I hope you’ll be able to escape it, too.
Stay safe in there!
 A new treatment could restore some mobility in people paralyzed by strokes
A new treatment could restore some mobility in people paralyzed by strokes 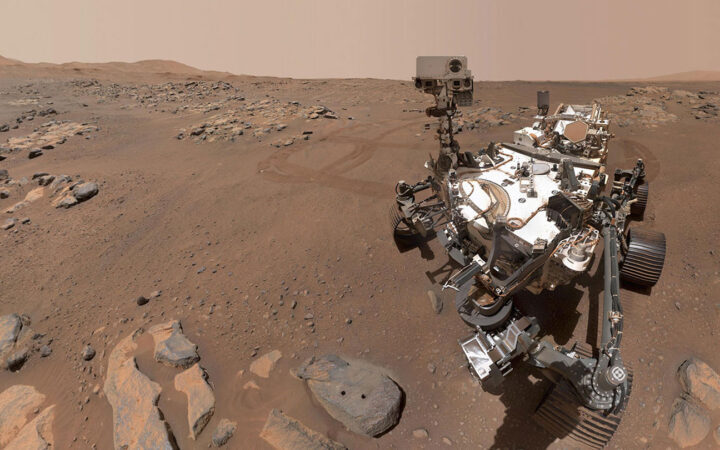 What has Perseverance found in two years on Mars?
What has Perseverance found in two years on Mars? 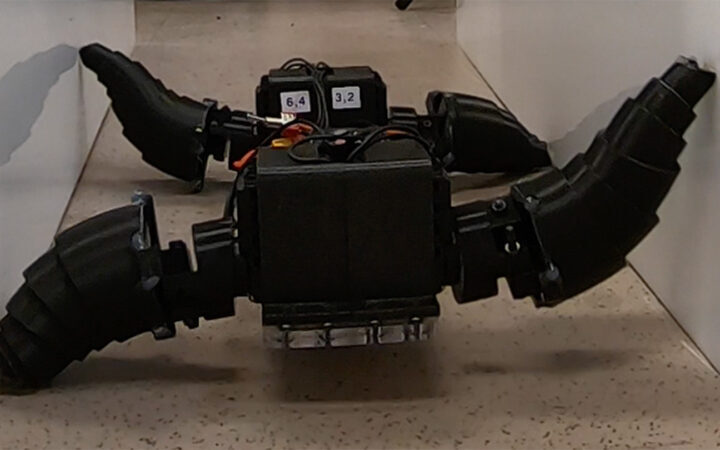 This robot automatically tucks its limbs to squeeze through spaces
This robot automatically tucks its limbs to squeeze through spaces  Greta Thunberg’s new book urges the world to take climate action now
Greta Thunberg’s new book urges the world to take climate action now  Glassy eyes may help young crustaceans hide from predators in plain sight
Glassy eyes may help young crustaceans hide from predators in plain sight 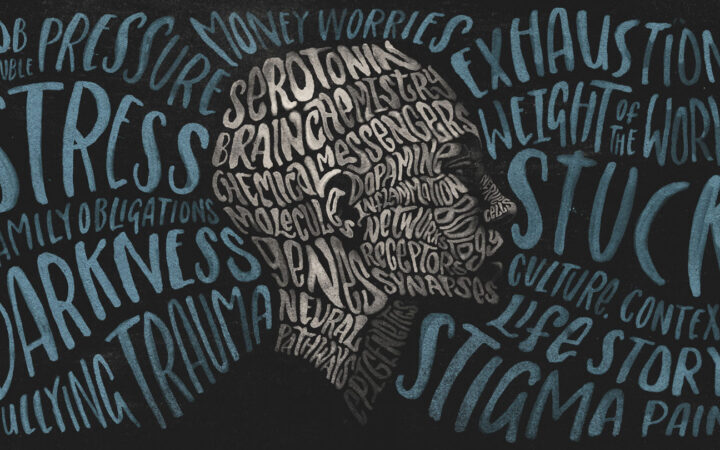 A chemical imbalance doesn’t explain depression. So what does?
A chemical imbalance doesn’t explain depression. So what does?